We all have resistance to change. It’s scary and unknown and we are creatures of habit, routine and comfort. The habitual brain is actually part of a survival technique. If we had to truly think through every step of everything we do each day as if it were our first time doing it, we wouldn’t get anything done. If you haven’t read The Power of Habit by Charles Duhigg, I strongly suggest you do.
data-animation-override>
“We need not only skills-based health education, but skills-progression health education.”
Many best practices or updated lessons don’t get implemented as a result of many reasons:
• Teachers hardly receive the amount of professional development they need to guide new practices, try new things and develop innovative, relevant approaches.
• Teachers do not have the time or energy. Being a teacher is so emotionally and physically exhausting. I wore a pedometer when I taught and averaged 8 miles of steps in a day. That’s the physical exhaustion. The emotional stress of working with over 100 children with 100 different needs is a challenge, both rewarding and leaves you with not much else to give to planning, changing, adapting and innovating.
• Many teachers do not have the support due to a lack of job-alike positions. In many schools, there is one health or physical educator, not a whole team to collaborate with.
• Lack of funding to purchase evidence-based materials/curricula is rare/minimal.
• Systems are in place as a result of textbooks lobbyists that keep evidence-based curricula from even getting on the state adopted/approved lists (don’t get me going on that one!).
These reasons that prevent educators from excelling, innovating, varying their curricula are out of teachers hands in many cases. Although, if you’re the only health teacher at your middle school, the opportunity to engage on social media, watch webinars, listen to podcasts, read books can help with a decrease in isolation.
However, I want to focus on resistance to change. I’m talking about the teacher that teaches the same 10 tobacco prevention lessons for five years in a row without adapting, updating, or determining if the students need it the way it’s always been taught. In the business world, people adapt their approaches to marketing, processes, creating, communicating constantly. They have to, to make a profit. Teachers are held accountable, but it’s not a profit like a business. I mean, the health and education of students is, but even then, I think we can do better.
Teachers that teach health education sometimes give our profession a bad name. And, I hate saying that, because I want to embrace all of them and give them tons of PD and help them teach through the lens of effective practices. However, it’s true. So many teachers are still using old practices and teaching from textbooks (and trust me, I’ve reviewed all the ones ya’ll think are good- they aren’t. They are FULL of un-functional knowledge that students do NOT need to know in order to lead to behavior changes). The amount of content is ridiculous and unimportant. If you want students to drink more water, they do not need to draw their digestive system and color it in. If you want students to learn about the harm of secondhand smoke, they don’t need to know what the chemicals look like under a microscope or even, really, how to spell the chemical names. I’m not going to mention these textbooks by name, but let’s just say, none made the cut when reviewing for a State DOE (un-named) through the lens of comprehensive skill-based health education. Do they incorporate the skill-standards? Yes, many do. But, it typically looks like this at the middle and high school level- 11 pages of content and one skill activity at the end. That is NOT skills-based health education. There is no logical skill progression over the lessons in order. There’s no scope and sequence that tells, you, the teacher, when the skill is introduced, reinforced and mastered. There are rarely rubrics and performance checklists. So, I urge you to ditch the textbook, or encourage your district to not buy it in the future. Save the thousands of dollars and purchase something stronger. Or, develop something on your own.
Textbooks don’t allow you to actually make local data-driven curricular decisions. They are written with assumptions on what your students need to know, when they need to know it and how. I’m not suggesting teachers change everything at once. Maybe take one unit and really look at the skill you want to incorporate and use RMC Health’s Health Skills Models (trust me- these are awesome!) to look at your grade level band to determine what mastery looks like for that skill. Check out the rubrics that accompany that skill. And, build a unit using a progression of the skill (see the Health Skill Model- it outlines it out!) and use content (unit topic) as context for teaching the skill. In fact, I guarantee the skill practice is more important than the content taught.
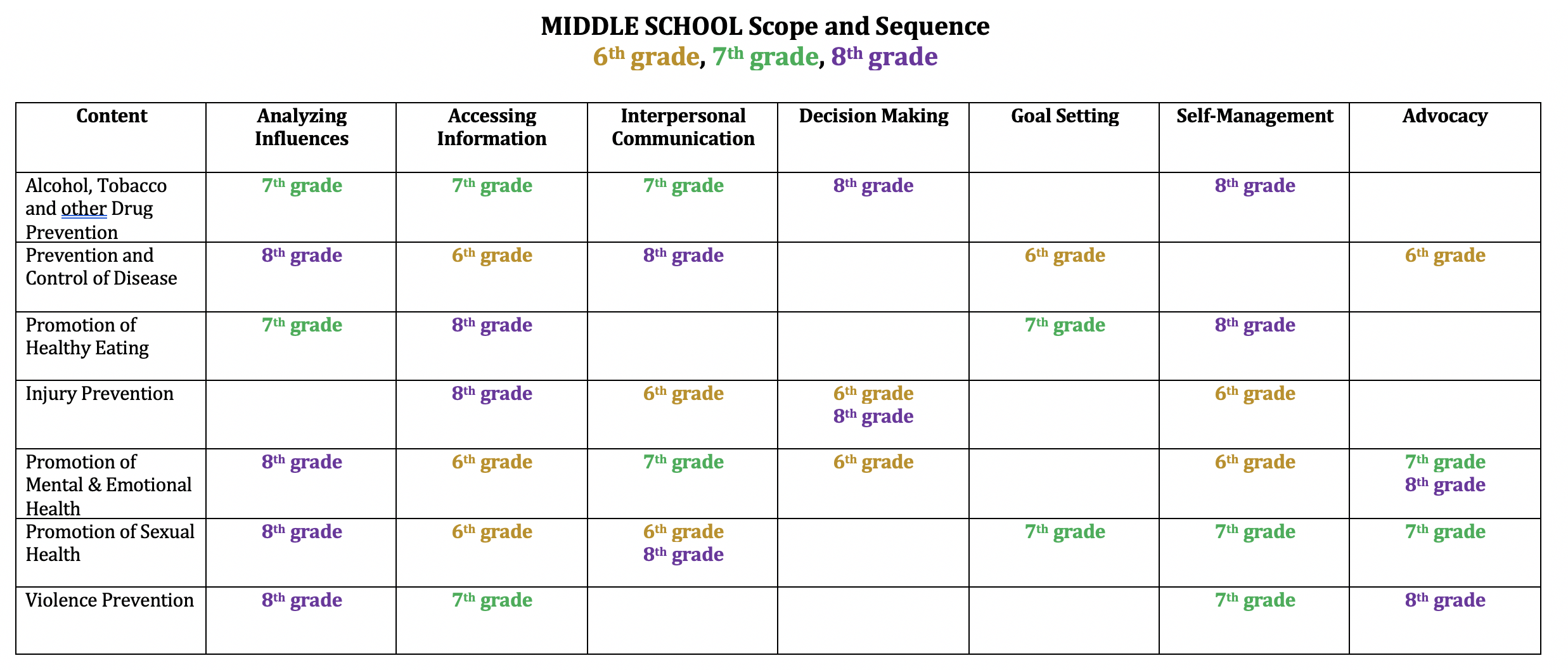
If you want to see an example of a high school unit with skill progression around analyzing influences- check this out. I wrote this unit (fee/accessible to all!) from the perspective of the unit being about the skill, not the content. So, I understand that may be a leap that’s too far for many of you, and that’s ok. Look at the 5 lessons and the assessment to see how much emphasis is put on the skill. Starting with the assessment (lesson 6) in mind, I developed the lessons to lead up to it. Lesson 1 begins here. There’s a menu at top to view the rest. I’m working on a middle school unit now- so stay tuned. Since I know it’s nice to have examples, here is the scope and sequence I’ve developed for middle school. This shouldn’t be your scope and sequence, since you need to use your own student data to inform when topics and skills should be taught. However, it’s an example.
So- as far as resistance to change… I’m not saying to teach all units through the skills lens versus content. I know as a field, we aren’t there and we don’t know if it actually works. However, I am asking that teachers push themselves to use local, county, state health YRBS data to drive what their students need, and focus on skills-progression. Not only skills-based health education, but skills-progression health education. What are the steps that students have the opportunity to practice multiple times through a planned scaffolding approach? Consider that and see where there might be gaps in your program!

I enjoy reading your blogs and this one in particular hit home. I worked in a district where the principal’s approach was "use the textbook." I didn’t even have enough of them for the 40 kids in my health class and I had this ridiculous ATOD program that would have taken me 200 minutes per week per grade level to implement (I saw kids 80 minutes per week for one-half of the year). I was secure enough to do my own thing and create my own reality. By doing so, I actually put my employment in jeopardy. Sometimes the "resistance" to change is simply a teacher following the local curriculum which has not been updated in 10 years due to budget and priorities. The "supervisor" may have no idea what constitutes quality skill-based health education and may focus on what is mandated in that district or state. For example, a teacher may simply be told to make sure you get in 15 hours of ATOD education because that is what the state will monitor and the teacher’s evaluation is based on completing those requirements. There is no incentive to change the curriculum, the programs used, or teaching practices. And this begins at the national level where we often create unrealistic topical health programs for teachers–and at the state level where we value hours and not quality or effectiveness. Effective teaching and learning requires administrators who support innovation and who recognize the value of health education as part of a whole child approach. We talk about creating school health champions–maybe we need to do a better job producing administrators who will champion what is best for kids–and who will support teachers to take risks and try new things rather than focusing on what is required and necessary. I firmly believe that teacher and administrator education must be changed in order for kids to succeed.
Linda,
I cannot agree more. I am perplexed at what to do in my situation. I teach sixth, seventh, and eighth grade classes. I get them for 40 minutes a day for 9 weeks. I may get some kids each year but there are many that only get it one of the three years. I try and update and make it skills based but that scope and sequence seems so unrealistic to me. I am a team of one- my administration really couldn’t care less what I teach- so that is a positive. I basically teach them what health is in sixth grade with a focus in mental/emotional and social health. In seventh grade we cover substance abuse (Emphasis in Tobacco/Juul, Marijuana, Alcohol). In eighth grade we focus on healthy living/nutrition. In all three grades I am required (school board) to have a Abstinence Ed group present for 4 of the classes (eye-roll), and then I usually take three extra days for damage recovery and have a pretty great sex ed discussion based lesson where they are able to ask whatever they want. My biggest problem is that I really love health- and my students and I try and get in as much as I can in such a short amount of time. I just wish I could figure out what the best things to do each day are- I do get stuck "rinse and repeating" which I hate. I know I do some things that really stick with these kids but I also know it could be better but really don’t know where to start…. so then I just go back to doing what I have been doing, granted I do edit and modify often. My problem is I do feel alone on an island with nobody to work with or collaborate with. I am the only health teacher in the building and the high school health teacher doesn’t have much interest in changing or even discussing… Any thoughts, Ideas, or advice would be helpful!
This is great! I am working slowly to transition our curriculum to skills-based but it is difficult as I am a one person team! I am presenting to my board next week and would love to share this scope and sequence as a sample of what I am trying to do.
This skills-based approach MUST be adopted by all who have responsibility for teaching Health and Physical Education. In addition, we must look for ways to extend the learning beyond the school day/curriculum into the families and communities. Obviously, the WSCC model opens the door for this to take place. Yet, for the WSCC model to be implemented effectively, each school district must have a HIGHLY-FUNCTIONING and ADMINISTRATIVELY SUPPORTED School District Wellness Council. All to often the WSCC model continues to focus on the 10 component areas, and not enough on the five Tenets and the Policies, Processes and Programs FUNCTION of the SCWC. Further, virtually every district has a learning platform that can be used effectively to personalize and complement any classroom learning. Using blended learning, there are incredible opportunities for teachers to create CHALLENGING (WSCC) and ENGAGING (WSCC) learning programs to allow for deep learning, project-based learning, and interactive learning, whether it the interactions be between teacher and student, student and student, student and parent, teacher and parent, student and community resource connections, or teacher and community resource connections. Though blended learning takes considerable time to establish the framework that personalizes and challenges all learners, and daily time to monitor, review and assess, the opportunity to bring about lifestyle change is worth it.
One further comment – why does the scope and sequence not include Promoting Physical Activity? Though this is often the focus of Physical Education classes, I feel it is a necessary reinforcer to focus on the protective factors and risk factors associated with physical inactivity and physical activity.
Hi Tom! This is an example- I suggest every school develops their own S+S based in data. In my example, there is a PE class that covers that PA components since Health Ed has so little time to cover everything else. In a perfect world, yes- there would be a content area around Promoting PA. But- this is just an example based on the simulated data from a community (with not many PA risk behaviors since they have a QPE program).
It’s as though this blog post was written just for me! I am currently struggling in a broken system. In a department with 8 other teachers, 4 of whom will be retiring in the next 5 years, I’m stuck. They are resistance to change- and we are part of a community that does not value our content- but quite frankly, why should they? As a whole, we have not provided valuable educational experiences for their children. I’m finding myself stuck in that space between wanting to initiate change, fighting for what I believe the students of our community deserve- and battling the habitual laziness and poor supervision that has been the HPE program at our high school for at least 2 decades. Do you have any suggestions or resources to help begin the process of advocating for change among my colleagues and the community?
Do you attend your State SHAPE Association’s conference or SHAPE America’s Speak Out Day? Be a member if not and there are opportunities for advocacy there. Also- SHAPE America’s page has a great Appropriate Practices in health Ed doc that is useful!
Thank you so much! I do not attend the SHAPE conference- but have started to expand my networking through social media- Twitter in particular.
There has been public discussion at board meetings and beyond about the ineffective structure of our current Health curriculum and we will be undergoing a complete program review. The superintendent and the associate superintendent of curriculum have asked for any suggestions of research based curriculum for Health- can you recommend any? I love the idea of skill-based, and would really love to see it in action and speak to professionals who have successfully made the transition.
Let me know if there is anything or anyone you would recommend.
THANK YOU!!!!
You might want to email me- jess@cairnguidance.com